|
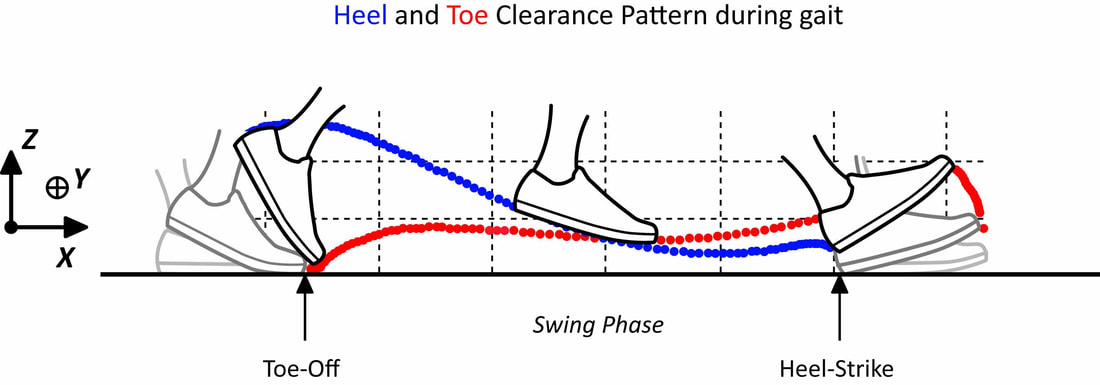
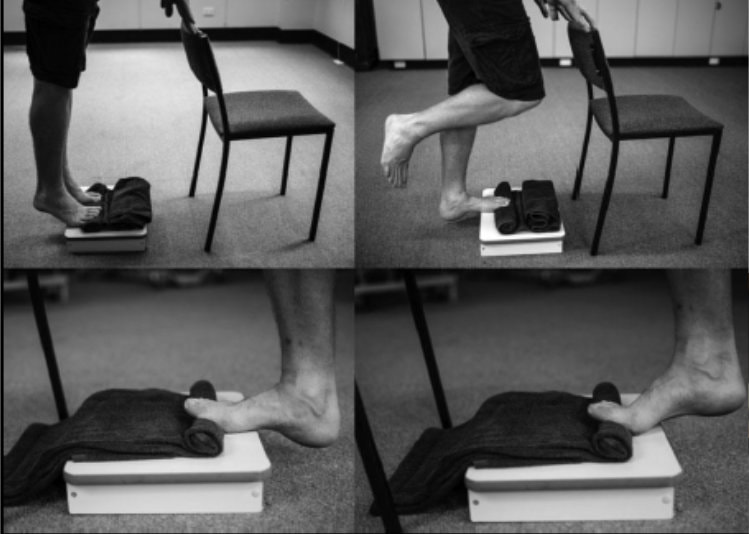
Let’s cut to the chase - if you have an ankle equinus (lack of ankle dorsiflexion) it means that you have an increased chance of developing retracted toes. The greater the equinus the more chance your toes will retract upwards (Cheuy et al., 2015). Your toes retract upwards through increased activity of the extensor muscles (extensor digitorum/hallucis longus/brevis) in response to the restriction in ankle range (most likely due to a short calf). Luckily these extensor muscles do work harder otherwise people with reduced ankle range would trip over their toes during the swing phase of gait. Ground clearance during swing phase is not very large (less than 2 cms for most people depending on height) (Winter, 1992). The downside of the increased extensor activity is it causes greater and greater hyperextension of the MTPJs and makes it harder for the intrinsics to keep the toes straight. During propulsion the lumbricals and interossei become ineffective in stabilising the toes and all we have left are the extrinsic flexors (Flexor digitorum longus which causes the toes to claw without the work of the intrinsics). Therefore, to stop this process we can’t just focus on intrinsic muscle strengthening. The fault in many cases can be the reduced range at the ankle joint (especially in diabetes). For the most part, patients with this limitation primarily have calf weakness and subsequent shortening (they go hand in hand e.g. if you immobilize the calf, it weakens and shortens itself to maintain a healthy length-tension relationship) (DiGiovanni et al., 2002). In diabetes the restriction is in combination with AGE’s (Advanced Glycation End products) which essentially decreased the flexibility of collagen (Rao et al., 2006). To get the best and most effective result for our patients we need to ask them to strengthen their calf muscles by performing an eccentric calf loading program. Eccentric strengthening of muscles in a lengthened position promotes greater strength and length by promoting the physiological process of sarcomerogenesis (Lynn and Morgan, 1994), essentially a process by which the muscle makes itself longer by adding on sarcomeres in series. Once you have done exercise in this way for a few months you will end up with an increased muscle resting length which will return some if not all the lost range in the ankle joint. In doing so you have reduced the need for the extensor muscles to work so hard to clear the ground. In return the patient will have improved range and power in propulsion which will have added benefits for hip and knee function. This is also by far a more effective program than stretching the calf muscles which will only offer short term benefits. Essentially using the ToePro to perform calf eccentric exercises combined with the intrinsic strengthening aspect will give patients a very effective approach to maximising their potential to improve range and improve toe alignment and strength. When do we call it quits? The problem that will raise its head very quickly for patients is that if they have walked in this way for a long period of time the flexion deformity they have developed in their toes may have become fixed. The calf exercises will still be effective in improving the ankle range if the equinus is due to the tightened calf muscles. It will also reduce the risk of further progression of the deformity and should therefore be recommended and most likely will benefit more proximal joints. It would not be unreasonable to recommend stretching of the shortened extensors passively (by say the hands, or by sitting on top of your feet with your feet maximally plantarflexed beneath you) or even to recommend strengthening the extensor tendons in a lengthened position also. The practitioner can also perform mobilisation and manipulation of both the ankle and toes to improve their range. References Cheuy, V. A. et al. (2015) ‘Muscle and Joint Factors Associated with Forefoot Deformity in the Diabetic Neuropathic Foot’, Foot and Ankle International, 37(5), pp. 514–521. doi: 10.1177/1071100715621544. DiGiovanni, C. W. et al. (2002) ‘Isolated gastrocnemius tightness’, Journal of Bone and Joint Surgery - Series A, 84(6), pp. 962–970. doi: 10.2106/00004623-200206000-00010. Lynn, R. and Morgan, D. L. (1994) ‘Decline running produces more sarcomeres in rat vastus intermedius muscle fibers than does incline running.’, Journal of applied physiology (Bethesda, Md. : 1985), 77(3), pp. 1439–1444. doi: 10.1152/jappl.1994.77.3.1439. Rao, S. R. et al. (2006) ‘Increased passive ankle stiffness and reduced dorsiflexion range of motion in individuals with diabetes mellitus’, Foot and Ankle International, 27(8), pp. 617–622. doi: 10.1177/107110070602700809. Winter, D. A. (1992) ‘Foot Trajectory in Human Gait: A Precise and Multifactorial Motor Control Task’, Physical Therapy. Oxford University Press, 72(1), pp. 45–53. doi: 10.1093/ptj/72.1.45.
2 Comments
The creator of the ToePro Dr Tom Michaud has released his own paper on the management of heel pain (plantar fasciitis).
"Each year, nearly 2 million Americans seek medical attention for a painful heel. In the US alone, the annual economic cost for managing this common condition is in excess of $300 million. Until recently, it was believed the most common cause of heel pain was an over-pronated foot...." Read the full article here. INCREASING STRENGTH OF INTRINSIC FOOT MUSCLES IN DIABETES WITH PERIPHERAL NEUROPATHY One component of diabetic foot disease is intrinsic muscle wasting – when it is present it is often referred to as the "intrinsic minus foot". The intrinsic minus foot is often discussed as an end stage change which occurs because of, or in addition to, long standing neuropathy and peripheral arterial disease. So, in the minds of many practitioners it is viewed as an inevitable, unfortunate change which sits at the top of a number of other problems in the latter stages of diabetic foot disease. In fact, intrinsic atrophy is one of the earliest changes in diabetic foot disease, occurs often long before peripheral neuropathy and vascular disease and is possibly one of the most important and now known to be reversible changes in the diabetic foot (Greenman et al., 2005; Höhne et al., 2012). However, in the minds of both practitioners and patients they are often more worried about peripheral neuropathy and vascular disease than muscle and structural changes. They often believe that these are the changes that herald the major risk for diabetic ulceration.
This is not the case for majority of people with diabetes. We know that the structural changes in the foot are significant predictors of ulceration and in fact are the predominant changes which lead to ulceration for most people (Holewski et al., 1989; Mueller et al., 2003). Essentially the structural changes in the foot – stiffening and clawing of toes - predict the high pressures under the forefoot. Without these changes you are unlikely to get the high forces which crush and injure foot tissues. If this is combined with a loss of sensation so you are unable to feel the crushing, or if you have a significant reduction in blood supply you cannot repair the crushed tissues. These later problems then escalate the risk significantly. To put it another way, if a patient does not develop stiffening and clawing of toes then they do not have the same level of crushing forces under their foot and if these forces are absent it is less of a concern when the patient develops neuropathy or a lack of blood supply. Our biggest priorities as practitioners is to do everything in our power to educate patients to begin the process of maintaining strength and mobility, especially of the toes, so they stop or reduce their risk of developing high forefoot pressures (Sartor et al., 2014). There is now a growing body of research which demonstrates we can indeed reverse muscle atrophy in the forefoot, improve mobility of toes and when we do so we can reduce plantar pressures which crush the tissues under the foot (Allet et al., 2010; Sartor et al., 2014; Kanchanasamut and Pensri, 2017). An excellent example of such research was published by Höhne et al in Cologne, Germany (Höhne et al., 2012). Fourteen diabetic patients with only 30% of normal toe flexor strength performed toe flexor training with 70% of the maximal voluntary isometric contraction on for eight weeks, 3 days per week, 4 sets per session for twelve repetitions (3s loading/ 3s relaxation). The participants were divided into groups of either those with or without neuropathy. Seven had neuropathy, seven without neuropathy. The maximum strength of the toes was measured before and after the intervention and the volume of the intrinsic foot muscles was examined before and after the intervention using MRI. All patients improved strength, with the average increase being a staggering 55% increase in just 8 weeks. The intervention took only 10 minutes roughly 3 times per week and could be performed at home with little difficulty. In addition, there were no instructions to utilise their strength in everyday activities. So the strength gains can only be attributed to intervention of a total of 30 minutes per subject per week. Furthermore, the MRI results showed an average increase of 5% muscle bulk in just those 8 weeks. We can begin to understand the possible benefits if we were to perform these exercises every day, in a functional position, with functional loads (bodyweight) combined with daily use activities to create positive carry over. References Allet, L. et al. (2010) ‘An exercise intervention to improve diabetic patients’ gait in a real-life environment’, Gait and Posture. Elsevier B.V., 32(2), pp. 185–190. doi: 10.1016/j.gaitpost.2010.04.013. Greenman, R. L. et al. (2005) ‘Foot small muscle atrophy is present before the detection of clinical neuropathy.’, Diabetes care. American Diabetes Association, 28(6), pp. 1425–30. doi: 10.2337/DIACARE.28.6.1425. Höhne, A. et al. (2012) ‘Increased Strength of Intrinsic Foot Muscles in Diabetes and Peripheral Neuropathy’, Journal of Biomechanics. Elsevier Ltd, 45(1), p. S201. doi: 10.1016/S0021-9290(12)70202-6. Holewski, J. J. et al. (1989) ‘Prevalence of foot pathology and lower extremity complications in a diabetic outpatient clinic.’, Journal Of Rehabilitation Research And Development, 26(3), pp. 35–44. Available at: http://www.ncbi.nlm.nih.gov/pubmed/2666642. Kanchanasamut, W. and Pensri, P. (2017) ‘Effects of weight-bearing exercise on a mini-trampoline on foot mobility, plantar pressure and sensation of diabetic neuropathic feet; a preliminary study’, Diabetic Foot and Ankle. Taylor & Francis, 8(1). doi: 10.1080/2000625X.2017.1287239. Mueller, M. J. et al. (2003) ‘Forefoot structural predictors of plantar pressures during walking in people with diabetes and peripheral neuropathy’, Journal of Biomechanics, 36(7), pp. 1009–1017. doi: 10.1016/S0021-9290(03)00078-2. Sartor, C. D. et al. (2014) ‘Effects of strengthening, stretching and functional training on foot function in patients with diabetic neuropathy: Results of a randomized controlled trial’, BMC Musculoskeletal Disorders, 15(1), pp. 1–13. doi: 10.1186/1471-2474-15-137.
Drs. Tom Michaud, Matt Dilnot, and Karen Mickle discuss the importance of toe strength. READ THE ARTICLE HERE. In addition to providing targeted treatment for intrinsic muscles of the foot, practitioners are now able to measure strength before, during and after treatment to ensure effective therapy.
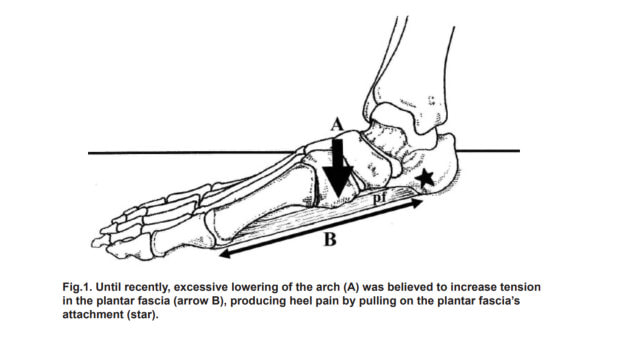
The Toe Strength Dynamometer is the first low cost and easily available instrument to assist in the measurement of foot strength in all people, including those with diabetes. The instrument evolved from the research of Professor Hylton Menz at La Trobe University in 2006 who sought to identify a simple method of measuring foot strength in a clinical setting using the age-old Paper Grip test (Menz et al., 2006). Leading author and respected biomechanics expert Dr Thomas Michaud adapted this technique to create the Toe Strength Dynamometer (Product name – ToePro Dynamometer™). Toe grip strength has been shown to detect foot muscle weakness and can predict risk of falls (Menz, Morris and Lord, 2006; Mickle et al., 2009), reduced athletic performance (Kulmala et al., 2014; Paquette, Devita and Williams, 2018), clawing of the toes (Mickle et al., 2009), and has been implicated in heel pain development (Sullivan et al., 2015; Barnes et al., 2017) and knee pain (Uritani et al., 2017) amongst other conditions. Identifying weakness and measuring response to physical therapy objectively has been difficult in a clinical setting. The Toe Strength Dynamometer gives practitioners the opportunity to solve this problem and measure physical therapy interventions for a variety of conditions in both diabetes and in a wide variety of other ailments of the lower limb. The Toe Strength Dynamometer can be used quickly and simply to create reliable, reproducible tests of foot strength and can be used as part of a standard foot assessment. With the identification of foot weakness practitioners can implement foot strength and mobilisation programs to assist in reversing the loss of strength and to maintain mobility of the forefoot (Balducci et al., 2006; Sartor et al., 2014; Kanchanasamut and Pensri, 2017). References Balducci, S. et al. (2006) ‘Exercise training can modify the natural history of diabetic peripheral neuropathy’, Journal of Diabetes and its Complications, 20(4), pp. 216–223. doi: 10.1016/j.jdiacomp.2005.07.005. Barnes, A. et al. (2017) ‘Clinical and Functional Characteristics of People With Chronic and Recent-Onset Plantar Heel Pain’, PM and R. American Academy of Physical Medicine and Rehabilitation, 9(11), pp. 1128–1134. doi: 10.1016/j.pmrj.2017.04.009. Kanchanasamut, W. and Pensri, P. (2017) ‘Effects of weight-bearing exercise on a mini-trampoline on foot mobility, plantar pressure and sensation of diabetic neuropathic feet; a preliminary study’, Diabetic Foot and Ankle. Taylor & Francis, 8(1). doi: 10.1080/2000625X.2017.1287239. Kulmala, J. et al. (2014) ‘Which muscles compromise human locomotor performance with age ? Which muscles compromise human locomotor performance with age ?’ Menz, H. B. et al. (2006) ‘Plantarflexion Strength of the Toes: Age and Gender Differences and Evaluation of a Clinical Screening Test’, Foot & Ankle International, 27(12), pp. 1103–1108. doi: 10.1177/107110070602701217. Menz, H. B., Morris, M. E. and Lord, S. R. (2006) ‘Foot and Ankle Risk Factors for Falls in Older People: A Prospective Study’, The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 61(8), pp. 866–870. doi: 10.1093/gerona/61.8.866. Mickle, K. J. et al. (2009) ‘ISB Clinical Biomechanics Award 2009. Toe weakness and deformity increase the risk of falls in older people’, Clinical Biomechanics. Elsevier Ltd, 24(10), pp. 787–791. doi: 10.1016/j.clinbiomech.2009.08.011. Paquette, M. R., Devita, P. and Williams, D. S. B. (2018) ‘Biomechanical Implications of Training Volume and Intensity in Aging Runners’, Medicine and Science in Sports and Exercise, 50(3), pp. 510–515. doi: 10.1249/MSS.0000000000001452. Sartor, C. D. et al. (2014) ‘Effects of strengthening, stretching and functional training on foot function in patients with diabetic neuropathy: Results of a randomized controlled trial’, BMC Musculoskeletal Disorders, 15(1), pp. 1–13. doi: 10.1186/1471-2474-15-137. Sullivan, J. et al. (2015) ‘Musculoskeletal and activity-related factors associated with plantar heel pain’, Foot and Ankle International, 36(1), pp. 37–45. doi: 10.1177/1071100714551021. Uritani, D. et al. (2017) ‘Relationship between toe grip strength and osteoarthritis of the knee in Japanese women: A multi-centre study’, Physiotherapy (United Kingdom), 101(25870971), pp. eS1560-eS1561. doi: http://dx.doi.org/org/10.1016/j.physio.2015.03.1559. The patented ToePro strengthening device facilities the most effective and simple method of improving foot muscle strength, can be used for effective eccentric calf exercises, promotes ankle flexibility and assists in strengthening synergists of the triceps surae complex. This device paves the way for practitioners now to focus on improving ankle flexibility and promoting strengthening of the muscles of the foot. This can potentially reduce and redistribute loads away from the plantar fascia and potentially improve strength for the outside stabilizers of the ankle. These are now considered to be significant contributors to the cause of heel pain in recent research by Barnes et al. (Barnes et al., 2017) Flexor hallucis longus, a forgotten but significant muscle with a tendon a fifth the size of the Achilles, exerts force of about 50% of bodyweight during propulsion (Jacob, 2001) and will likely also improve better control of motions of the foot and ankle and reduce loads on the plantar fascia. The authors of the paper by Barnes et al from Sydney University make the following statement regarding foot strength in their discussion: “Toe flexor and ankle eversion strength was reduced in the plantar heel pain group, ……. Toe flexor weakness has been previously identified in a small sample of people with plantar heel pain, and our larger study provides further evidence that toe flexor weakness may be associated with plantar heel pain. “ Although this paper refers to only one other study with a “small sample size”, conducted by Allen and Gross in 2003, in fact there are other studies that have also identified intrinsic muscle atrophy with heel pain. This includes a study by Chang et al 2012 who found intrinsic muscle atrophy in the forefoot was associated with heel pain; Cheung et al 2016 found rearfoot intrinsic atrophy was associated with heel pain; and additionally, Wearing in 2004 also implied the involvement of foot intrinsic muscles was required to potentially offload the plantar fascia (Allen and Gross, 2003; Wearing et al., 2004; Chang, Kent-Braun and Hamill, 2012; Cheung et al., 2016). References Allen, R. H. and Gross, M. T. (2003) ‘Toe flexors strength and passive extension range of motion of the first metatarsophalangeal joint in individuals with plantar fasciitis.’, The Journal of orthopaedic and sports physical therapy, 33(8), pp. 468–78. doi: 10.2519/jospt.2003.33.8.468. Chang, R., Kent-Braun, J. A. and Hamill, J. (2012) ‘Use of MRI for volume estimation of tibialis posterior and plantar intrinsic foot muscles in healthy and chronic plantar fasciitis limbs’, Clinical Biomechanics. Elsevier Ltd, 27(5), pp. 500–505. doi: 10.1016/j.clinbiomech.2011.11.007. Cheung, R. T. H. et al. (2016) ‘Intrinsic foot muscle volume in experienced runners with and without chronic plantar fasciitis’, Journal of Science and Medicine in Sport, 19(9), pp. 713–715. doi: 10.1016/j.jsams.2015.11.004. Jacob, H. A. C. (2001) ‘Forces acting in the forefoot during normal gait - An estimate’, Clinical Biomechanics, 16(9), pp. 783–792. doi: 10.1016/S0268-0033(01)00070-5. Wearing, S. C. et al. (2004) ‘Sagittal movement of the medial longitudinal arch is unchanged in plantar fasciitis.’, Medicine and science in sports and exercise, 36(10), pp. 1761–7. doi: 10.1249/01.MSS.0000142297.10881.11. Research conducted in Sydney, Australia has clarified what has been suspected by a growing number of researchers around the world as major contributors to the cause of plantar fasciitis (heel pain). The research identified that limited ankle range, reduced foot (toe flexor) and leg strength (peroneal strength) and increased bodyweight appear to play a significant role in this condition (Barnes et al., 2017). The study conducted at Sydney University involved several leaders in musculoskeletal research. The research was significant for both the quality as well as the breadth of the research that was conducted. The study compared 71 people with long term heel pain with 61 people who had heel pain of less than 6 months. This world leading research group used this 2017 publication to extend on the research they published in 2015 in which 202 people with heel pain were compared with 70 well matched controls. Both papers evaluated an extensive range of factors (outlined below) to isolate which of these appear to be the most important in clinical assessment and treatment. The factors evaluated have at various times been implicated in the development of heel pain but required further research. The factors included: Biomechanical alignment; joint mobility; muscle strength of both the foot and leg; calf endurance; and weightbearing activity levels. Importantly this research has clarified what is not likely to be important in plantar fasciitis. Specifically heel pain was not associated with big toe range of motion (either high or low flexibility); excessive flexibility of the arch (hypermobility); calf strength or calf endurance; inwards or outwards movement of the foot; foot alignment; occupational standing time, or exercise level. Interestingly it has shined a light on the work of Rathleff et al. in 2009 which appeared to indicate that high load strength training for the calf muscles was an effective treatment for plantar fasciitis. The new research from Barnes proved this unlikely to be the case indicating both calf strength and endurance were not associated with heel pain risk. The research by Rathleff has been criticised previously. Specifically, it was criticised for its methodology which a) combined multiple treatments at once but singled out high load calf strengthening as the over-riding effective treatment b) had no control group and c) showed that strengthening took a very long time to take effect in respect to normal clinical practice i.e. 3 months and d) the groups were only different at the 3 month point and in fact the strength group were slightly, but not statistically significant, worse at the end of the study than the non-strength group (Rathleff et al., 2015). Only the non-strengthening group had subjects who reported no pain at the 12-month point. Interestingly, the natural history of plantar fasciitis even without treatment has been suggested to be 12 months (Caselli et al., 1997). However, there are important aspects to the Rathleff study. The calf exercises in the study are done through a full range and involve eccentric loading. This is likely to be an effective way of maximising flexibility of the ankle, in keeping with the new research paper which suggested that reduced ankle range may be of significance as a cause of plantar fasciitis. Eccentric loading in a lengthened position is also likely to result in the addition of sarcomeres in series (sarcomerogenesis) to the calf muscle improving its resting length and therefore improving ankle range. These adaptations also potentially increases the joint angle at which peak torque is generated (O’Sullivan, McAuliffe and DeBurca, 2012). All of this is likely to improve better ankle control through its entire range, improve better control of forward body movement (especially in the case of increased BMI) and ultimately helps to unload the plantar fascia through the propulsive period of gait. Thus, asking patients to perform calf strengthening exercises on a step is likely to be helpful, especially through the full lower range, although we are unsure as to whether placing a towel under the toes whilst doing this is necessary. About heel pain Plantar heel pain is the most common foot disorder treated by health care practitioners (Martin et al., 2014). It occurs mainly in adults and effects people who come from both active and sedentary lifestyles. In the United States approximately 2 million people seek treatment for plantar heel pain every year, at a cost of more than $300 million (Riddle and Schappert, 2004; Tong and Furia, 2010). Heel pain is believed to occur due to excessive cumulative strain at the attachment of the plantar fascia and mechanical overload is thought to play a major role in causing this condition. Best care of heel pain has alluded practitioners for decades with researchers in the past being unable to identify the likely causative factors. References Barnes, A. et al. (2017) ‘Clinical and Functional Characteristics of People With Chronic and Recent-Onset Plantar Heel Pain’, PM and R. American Academy of Physical Medicine and Rehabilitation, 9(11), pp. 1128–1134. doi: 10.1016/j.pmrj.2017.04.009. Caselli, M. et al. (1997) ‘Evaluation of magnetic foil and PPT Insoles in the treatment of heel pain’, Journal of the American Podiatric Medical Association, 87(1), pp. 11–16. doi: 10.7547/87507315-87-1-11. Martin, R. L. et al. (2014) ‘Heel Pain—Plantar Fasciitis: Revision 2014’, Journal of Orthopaedic & Sports Physical Therapy, 44(11), pp. A1–A33. doi: 10.2519/jospt.2014.0303. O’Sullivan, K., McAuliffe, S. and DeBurca, N. (2012) ‘The effects of eccentric training on lower limb flexibility: A systematic review’, British Journal of Sports Medicine, 46(12), pp. 838–845. doi: 10.1136/bjsports-2011-090835. Rathleff, M. S. et al. (2015) ‘High-load strength training improves outcome in patients with plantar fasciitis: A randomized controlled trial with 12-month follow-up’, Scandinavian Journal of Medicine & Science in Sports, 25(3), pp. e292–e300. doi: 10.1111/sms.12313. Riddle, D. L. and Schappert, S. M. (2004) ‘Volume of Ambulatory Care Visits and Patterns of Care for Patients Diagnosed with Plantar Fasciitis: A National Study of Medical Doctors’, Foot & Ankle International, 25(5), pp. 303–310. doi: 10.1177/107110070402500505. Tong, K. B. and Furia, J. (2010) ‘Economic burden of plantar fasciitis treatment in the United States’, American Journal of Orthopedics (Chatham, Nj), 39(5), pp. 227–231. |
AuthorMatt Dilnot is a Podiatrist working in the Eastern Suburbs of Melbourne, Victoria. Archives
May 2020
Categories |





 RSS Feed
RSS Feed