|
Drs. Tom Michaud, Matt Dilnot, and Karen Mickle discuss the importance of toe strength. READ THE ARTICLE HERE.
0 Comments
In addition to providing targeted treatment for intrinsic muscles of the foot, practitioners are now able to measure strength before, during and after treatment to ensure effective therapy.
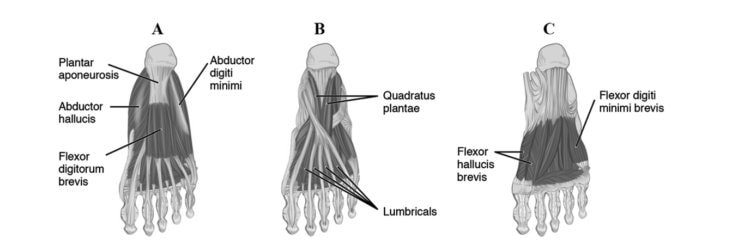
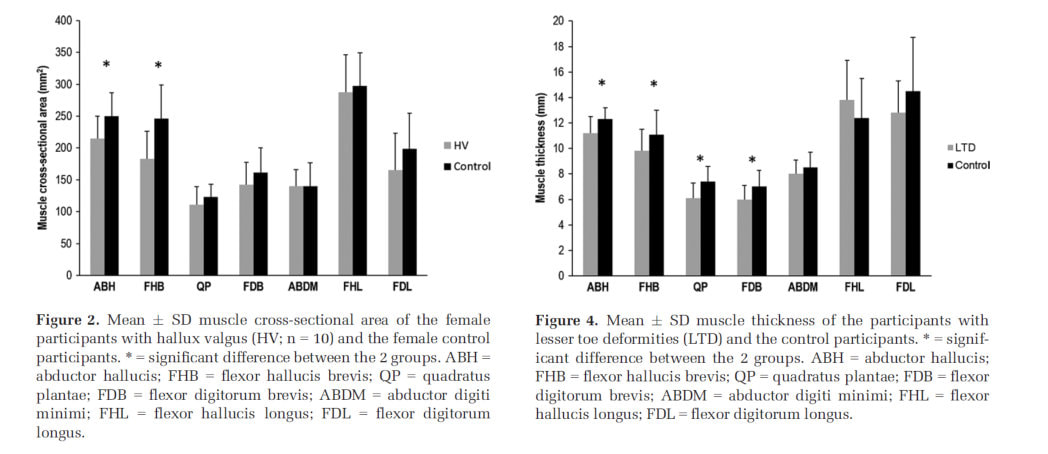
The Toe Strength Dynamometer is the first low cost and easily available instrument to assist in the measurement of foot strength in all people, including those with diabetes. The instrument evolved from the research of Professor Hylton Menz at La Trobe University in 2006 who sought to identify a simple method of measuring foot strength in a clinical setting using the age-old Paper Grip test (Menz et al., 2006). Leading author and respected biomechanics expert Dr Thomas Michaud adapted this technique to create the Toe Strength Dynamometer (Product name – ToePro Dynamometer™). Toe grip strength has been shown to detect foot muscle weakness and can predict risk of falls (Menz, Morris and Lord, 2006; Mickle et al., 2009), reduced athletic performance (Kulmala et al., 2014; Paquette, Devita and Williams, 2018), clawing of the toes (Mickle et al., 2009), and has been implicated in heel pain development (Sullivan et al., 2015; Barnes et al., 2017) and knee pain (Uritani et al., 2017) amongst other conditions. Identifying weakness and measuring response to physical therapy objectively has been difficult in a clinical setting. The Toe Strength Dynamometer gives practitioners the opportunity to solve this problem and measure physical therapy interventions for a variety of conditions in both diabetes and in a wide variety of other ailments of the lower limb. The Toe Strength Dynamometer can be used quickly and simply to create reliable, reproducible tests of foot strength and can be used as part of a standard foot assessment. With the identification of foot weakness practitioners can implement foot strength and mobilisation programs to assist in reversing the loss of strength and to maintain mobility of the forefoot (Balducci et al., 2006; Sartor et al., 2014; Kanchanasamut and Pensri, 2017). References Balducci, S. et al. (2006) ‘Exercise training can modify the natural history of diabetic peripheral neuropathy’, Journal of Diabetes and its Complications, 20(4), pp. 216–223. doi: 10.1016/j.jdiacomp.2005.07.005. Barnes, A. et al. (2017) ‘Clinical and Functional Characteristics of People With Chronic and Recent-Onset Plantar Heel Pain’, PM and R. American Academy of Physical Medicine and Rehabilitation, 9(11), pp. 1128–1134. doi: 10.1016/j.pmrj.2017.04.009. Kanchanasamut, W. and Pensri, P. (2017) ‘Effects of weight-bearing exercise on a mini-trampoline on foot mobility, plantar pressure and sensation of diabetic neuropathic feet; a preliminary study’, Diabetic Foot and Ankle. Taylor & Francis, 8(1). doi: 10.1080/2000625X.2017.1287239. Kulmala, J. et al. (2014) ‘Which muscles compromise human locomotor performance with age ? Which muscles compromise human locomotor performance with age ?’ Menz, H. B. et al. (2006) ‘Plantarflexion Strength of the Toes: Age and Gender Differences and Evaluation of a Clinical Screening Test’, Foot & Ankle International, 27(12), pp. 1103–1108. doi: 10.1177/107110070602701217. Menz, H. B., Morris, M. E. and Lord, S. R. (2006) ‘Foot and Ankle Risk Factors for Falls in Older People: A Prospective Study’, The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 61(8), pp. 866–870. doi: 10.1093/gerona/61.8.866. Mickle, K. J. et al. (2009) ‘ISB Clinical Biomechanics Award 2009. Toe weakness and deformity increase the risk of falls in older people’, Clinical Biomechanics. Elsevier Ltd, 24(10), pp. 787–791. doi: 10.1016/j.clinbiomech.2009.08.011. Paquette, M. R., Devita, P. and Williams, D. S. B. (2018) ‘Biomechanical Implications of Training Volume and Intensity in Aging Runners’, Medicine and Science in Sports and Exercise, 50(3), pp. 510–515. doi: 10.1249/MSS.0000000000001452. Sartor, C. D. et al. (2014) ‘Effects of strengthening, stretching and functional training on foot function in patients with diabetic neuropathy: Results of a randomized controlled trial’, BMC Musculoskeletal Disorders, 15(1), pp. 1–13. doi: 10.1186/1471-2474-15-137. Sullivan, J. et al. (2015) ‘Musculoskeletal and activity-related factors associated with plantar heel pain’, Foot and Ankle International, 36(1), pp. 37–45. doi: 10.1177/1071100714551021. Uritani, D. et al. (2017) ‘Relationship between toe grip strength and osteoarthritis of the knee in Japanese women: A multi-centre study’, Physiotherapy (United Kingdom), 101(25870971), pp. eS1560-eS1561. doi: http://dx.doi.org/org/10.1016/j.physio.2015.03.1559.  At first glance, this study doesn't seem so surprising Fifteen men performed a heavy resistance toe flexor strength training program for their feet and ankles with 90% of their maximal voluntary isometric contraction for 7 weeks (560 contractions). At the end of the 7 week program push-off strength in the feet and ankles had more than doubled, toe strength had increased 10-15% and jump distance had increased on average about 7%.(Goldmann et al., 2013) On the face of it, it makes sense that performing high resistance training for your foot muscles would indeed be quite effective, if not a well established method of improving foot strength. That last part is where you would be wrong. It has not been a well established fact. In fact so few people considered it a possibility that almost no one has studied it. To date, there have been few attempts to measure and strengthen foot muscles while looking at changes in function. More specifically there are even fewer studies which look at the ability to specifically strengthen toe-flexor muscles and we have been somewhat sceptical that it would make the slightest difference. Further, of those that have attempted to do this before, the results have been somewhat disappointing (Spink, Fotoohabadi and Menz, 2010; Houck et al., 2017) which makes this study even more compelling. Previous studies had asked participants to exercise their muscles with loads and in positions that are not functional i.e. don't represent loads typical of those experienced when walking and in positions that don't represent how the joint is used during activities such as walking, running, jumping or sprinting. This study adds enormously to the rapidly growing research surrounding the importance of foot muscle strength. All people involved with rehabilitation, including those interested in foot, knee, hip and back function need to get with the program and grow their knowledge base. References Goldmann, J. P. et al. (2013) ‘The potential of toe flexor muscles to enhance performance’, Journal of Sports Sciences, 31(4), pp. 424–433. doi: 10.1080/02640414.2012.736627. Houck, J. et al. (2017) ‘Can Foot Exercises Alter Foot Posture, Strength, and Walking Foot Pressure Patterns in People with Severe Flat Foot?’, AOFAS Annual Meeting, pp. 1–2. doi: 10.1177/2473011417S000199. Spink, M. J., Fotoohabadi, M. R. and Menz, H. B. (2010) ‘Foot and ankle strength assessment using hand-held dynamometry: Reliability and age-related differences’, Gerontology, 56(6), pp. 525–532. doi: 10.1159/000264655. It is surprising how long it has taken for significant steps to be made in understanding the relationship between foot muscle strength and foot function. The most recent exciting paper has come from one of the world leaders in the research of intrinsic muscles and their implications in toe deformities. Karen Mickle from Victoria University, Australia has been extraordinarily productive over the last 10 years with her use of diagnostic ultrasound and dynamometers. She has collaborated with some well known researchers too including Chris Nester and Hylton Menz. The most recent paper to have come forth from Karen has just been published in Arthritis Care & Research. Essentially the results of this paper have confirmed what has long believed to be the case i.e. if you have toe deformities such as hallux valgus and claw toes, you are likely to have atrophic (smaller and weaker) muscles. If you have hallux valgus you have a smaller abductor hallucis, if you have lesser toe deformities (claw toes) then you had atrophy and weakness in the intrinsics attached to these. This study collected data from 44 older adults (>60 years) with either toe deformities or not (controls). They then underwent ultrasound assessment to look at the size of the muscles in their feet with a standardized protocol. What was particularly interesting in this study was that virtually every muscle examined (of which there were 7 different muscles examined) was atrophic relative to the controls, bar flexor hallucis longus. Take a look at the chart below: The tricky part of this research then leads us to the next important question. Does the atrophy occur because of the toe deformity or does it lead to the toe deformity? Current evidence would point to the latter, which suggests specifically in relation to hallux valgus that prevention through exercise should happen in the early stages to stop the progression of the deformity. Once the abductor hallucis muscle moves under the 1st metatarsal it acts as a weak flexor instead of an abductor.
References:
This interview with Dr Tom Michaud was conducted on 19th December 2017 with the "2 Movement Guys", Adam Wolf,PT and Nicholas Studholme, DC. It is an enjoyable general chat about orthoses, strength and some general lower limb management tips. "Interested in orthotics, biomechanics, and foot function? Check out the recent podcast with Dr. Tom Michaud D.C., author of Human Locomotion: The Conservative Management of Gait-Related Disorders, as used in physical therapy, chiropractic, pedorthic, and podiatry schools around the world. Tom is a wealth of clinically relevant and easily applicable information. This is going to be worth your time!" Podcast here: References in this Podcast include: Titanium rods and tibio-femoral rotation
Samuel Adams Beer - Boston Lager |
AuthorMatt Dilnot is a Podiatrist working in the Eastern Suburbs of Melbourne, Victoria. Archives
May 2020
Categories |




 RSS Feed
RSS Feed