|
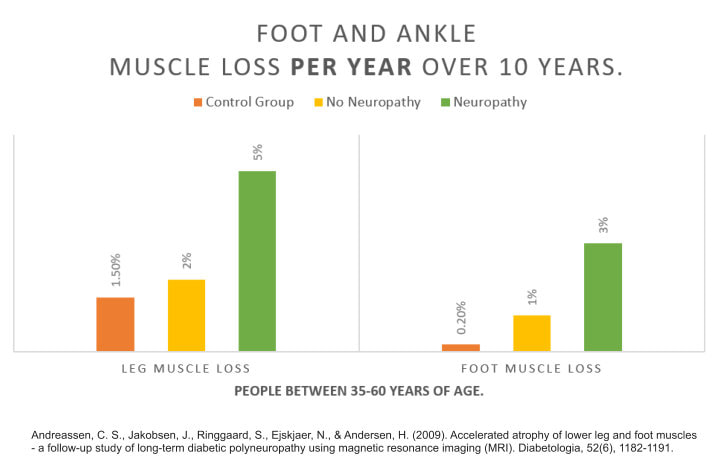
The understanding of ageing on muscle loss (called sarcopenia) has undergone rapid development over the last 50 years. Although we don't know all the reasons why people lose muscle mass as they age, most of the reasons are probably now known.1 As we age, the muscle loss is typically worse in the hands and feet, the latter causing issues with balance and tripping. Diabetes is known to accelerate the ageing process and the more poorly controlled the diabetes typically the worse the muscle loss.2 To quantify the amount of muscle loss a group of researchers looked at MRIs of the foot and ankle in images that were taken of the same people 10 years apart.3 To further investigate the results they divided the patients up broadly into those that had neuropathy, those that didn't have neuropathy and a healthy control group without any disease. The results can be seen in the following graph: Annual loss of foot and ankle muscle in people aged around 35 - 60 years. Comparing MRIs of patients feet, looking at the same muscles with an approximate 10 year gap in between.
Leg muscles: Neuropathic patients: About 5% of muscle lost each year. Non-neuropathic patients: About 2% loss of muscle each year. Controls: About 1.5% loss of muscle each year. Foot muscles: Neuropathic patients: About 3% of muscle lost per year. Non-neuropathic patients: About 1% lost per year. Controls: About .2% lost per year. Conclusions/interpretation: Muscular atrophy in long-term diabetic neuropathy occurs early in the feet, progresses steadily in the lower legs, relates to severity of neuropathy and leads to weakness at the ankle. Reference
1 Comment
The debate around whether or not we were designed to wear shoes has been around for a long time now and has particularly hotted up since the introduction of minimalist shoes in the early 2000's. What is defined as a minimalist shoes is quite difficult to work out. Is it a pair of flip-flops (jandals, thongs), which have been around since way before the hipster minimalist shoes came along? Certainly people run in them, if just for running for the bus or even in a marathon (yes, he does complete them in the one pair of shoes) . As it happens, to decide what features were important in determining a minimalist shoe an expert panel of 42 shoe boffins got together, did some number crunching and came up with a list of key features. Then to make it more useful they created a minimalist index system so shoes could be rated and then their respected result can be reported when it is used in a research paper e.g. this research used a minimalist shoe with an MI of 58 for example. To come up with the Minimalist Index for a shoe, you assign 0 to 5 points for each of the following categories: 1. Weight. 5 points for when the shoe weighs less than 125 grams (4.4 oz); 0 points for shoes weighing more than 325 grams (11.5 oz). 2. Stack height. This is the thickness of the sole at the center of the heel. Shoes less than 8mm are given maximum points and shoes over 32mm are given 0. 3. Heel to toe drop. Less than 1 millimeter is considered most minimalist and over 13 millimeters is considered a zero score. 4. Motion control and stability technologies. You start with five points, and lose one for every technology included in the shoe e.g. heel counter equals 1 point, mid-sole shank 1 point, board lasting 1 point, etc. 5. Flexibility. Half of the points (i.e. 2.5) are awarded for longitudinal flexibility, which is how much the shoe folds up when you press from the heel and toe. The other half is awarded to torsional flexibility, which is how much you can twist the shoe when you rotate the toe in one direction and the heel in the other. Add up all these points, and you get a score out of 25; multiply that score by four, and you get the Minimalist Index, ranging from 0 to 100. Some key points:
Shoe size: What is a rather bizarre aspect of this paper when you look in both the detailed MI guide or the rating scale, neither of them advise as to what size shoe you should be applying the test to. AS IT HAPPENS, IF YOU READ THE PAPER YOU WILL SEE THAT THE CONTRIBUTORS WERE GIVEN A SIZE US9 MENS SHOE TO EVALUATE. THIS IS NOT STATED IN THE MI GUIDES OR RATING SCALE. This is a frequent issue in research papers. Whenever you see measurements in mm and mg or inches and pounds rather than percentages, ratios and angles you should immediately be suspicious. In this case we don't need to be suspicious of the results but it would have been better to have given weights and measures as percentages, angles, ratios. Let's take for example an average men's and women's shoe.To define average you would normally take the running reference shoe being around size 9 US in both the women's and the men's. Immediately you have a problem because a women's 9 US is not a men's 9 US, they are different sizes. In addition, there isn't a universal perfect sizing system for footwear so one manufacturers sizing system can be different from another. Most of us have had the experience of shoes with the same size fitting quite differently. The different sizing will effect all of the measurements that are awarded a weight or a measure. So, in my case I take a size 12UK (13US). If I weigh my Nike Free in a size 13US it will be significantly heavier than the size 9. The stack height will be greater, the heel pitch will be higher and even the flexibility will be effected due to a combination of thicker materials and altered lever arms. It is difficult for me to work out where my shoe rates in this scale. If I was female and I contacted Nike for weights and heights in size US9 female for my model of shoe I would still have problems because women's 9 is not the same as men's 9. Trying to work out the MI calculations would still be quite difficult as I would somehow need to convert the mens US9 to an equivalent female size and then convert this to the size that I was wearing or wanting to use in my research. Natural function of the foot: One of the hardest aspects to determine in a minimalist shoe is whether or not it allows the "natural" function of the foot. There is an endless list of areas to discuss when it comes to this point. An example might be a pair of "thongs" versus a pair Vibram 5 fingers. The pair of thongs I would guess causes an "unnatural" running style versus the 5 fingers but we have to remember your "natural" running style is constantly altering to the surfaces, speed, fatigue, fitness, gradient of the ground, etc. All of these aspects vary from person to person. Any interface which protects or alters skin contact with the ground will alter your "natural" running style. Stimulating or dare I say "hurting" receptors in your skin in the forefoot will increase toe function and your entire lower limb mechanics, just watch anyone walking back to their car across a gravel car park barefoot. You can see it even effects their face as they carefully place their feet and recoil from the discomfort or sharp stones. Picture the same person walking back to their car with runners on. Which gait was more normal. Which one of those gaits was more efficient and less injurious to the joints. On the flip side, the person walking in barefoot across gravel regularly will strengthen parts of their body they would never strengthen with running shoes on. Equally they could also damage the structures permanently as well. Roll the dice on what you would prefer. So overall I like the intentions of this paper and I commend the authors and all those that participated. I think generally this guide is close enough to give us a rough guide, but the implementation in a research or personal situation could be rather clunky. Esculier, Jean-Francois, et al. "A consensus definition and rating scale for minimalist shoes." Journal of foot and ankle research 8.1 (2015): 42. This is some rather old information but it never surprises me as to how long it takes for information to move into the wider world of health education.
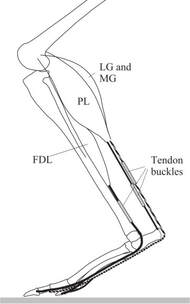
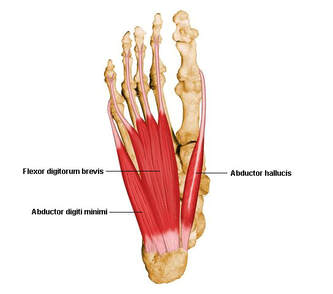
Following on from the previous great work by Dominic Farris et al. we have a new article which gives us insights into the contribution of 2 of the largest intrinsic muscles of the foot, abductor hallucis and flexor digitorum brevis. Specifically, this research attempts to unravel how much of the foots function is passive and how much contributes by muscular function. When humans walk it is well known that a significant amount of the energy for forward motion occurs through the use of passive (built-in) springs of the body. Essentially these springs, such as the achilles tendon and plantar fascia, can “catch” some of the energy of the body landing down on the ground, “stretches” like a rubber band and then recoils to return a lot of the energy collected to rise the body back up again. The achilles tendon of course is one of the most significant human springs during walking and especially running and provides a sort of “free” energy to these motions rather than meaning all energy for walking comes only from the “push” of muscles. It is said that both Turkey’s and Kangaroos can reach a locomotion pace where the spring in their legs returns most of the energy for forward movement and therefore they can continue moving at this pace very efficiently with very little oxygen consumed relative to their mass. The kangaroo of course does this with enormously long feet with an enormously long achilles tendon to capture the bounce energy and return it. This new research conducted by Ryan Riddick shows that the foot plays an important role in accelerating and decelerating the body during powerful movements and can contribute up to 20% of the power from the lower limb. This new research specifically set out to establish how much the muscles of the foot contribute to lower limb power versus power that is simply contributed from the passive or non-muscular tissues such as the ligaments and fascia. When pushing off and up from the ground such as when climbing stairs, hills, or jumping, the foot muscles contribute about 10% of the total leg power, which doesn’t sound like a lot, but at least 90% of the foots contribution occurs through the muscles of the feet rather than the passive structures. In this study only the two muscles abductor hallucis and flexor digitorum brevis were monitored and it is of course likely that muscular input will amount to more than what has been estimated in this study. It can be assumed that as has been found in other research, without adequate foot strength and muscle function more load is placed on the passive structures of the foot, particularly the plantar fascia. When decelerating the body, the feet are even more important where they contribute about 20% of deceleration force with around 30% of this occurring from foot muscle activity and the rest from passive structures. This could be related to any sport where agility is important. In order to be agile we need to be able to rapidly prevent our continued movement in one direction and quickly transition from braking force into propulsive force. Therefore, we can assume that for a lot of sports like basketball, football, soccer, etc. which require rapid changes in direction that foot strength is going to play a role. It also tells us that when we are decelerating in sport we are likely placing a lot of stress on the passive structures of the foot which will be offloaded by the work of the muscular tissues. Riddick, Ryan, Dominic J. Farris, and Luke A. Kelly. "The foot is more than a spring: human foot muscles perform work to adapt to the energetic requirements of locomotion." Journal of the Royal Society Interface 16.150 (2019): 20180680.
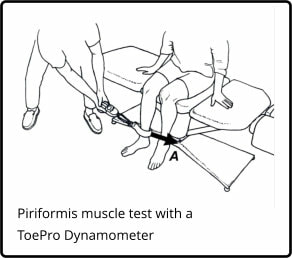
Seven percent of athletes who score less than 20% body weight will tear their ACLs each season.1
Recent research confirms that when piriformis strength is less than 20% body weight, the individual is significantly more likely to be injured. ACL tears are especially common when a weak piriformis is present. The ToePro/Hip Strength Dynamometer makes it easy to measure hip strength. An ankle strap attachment allows you to create a ratio between hip strength and body weight. Simply multiply the patients weight in kg by .2 to work out what minimum strength is and perform the test e.g. 80kg x .2 = 16kg.
Read the full article by Dr Thomas Michaud on hip strength and knee function here. Relatively new article in the National Academy of Sciences journal. Farris, Kelly, Cresswell and Lichtwark I believe have written a wonderful paper clarifying the role of the intrinsic muscles of the foot.
Farris, D. J. et al. (2019) ‘The functional importance of human foot muscles for bipedal locomotion’, Proceedings of the National Academy of Sciences, p. 201812820. doi: 10.1073/pnas.1812820116. The conclusion has an especially important comment: "In conclusion, we have shown that the PIMs (Plantar Intrinsic Muscles) actively contribute to stiffening of the MTP joint in late stance during walking and running, to assist propulsive push-off, and that the windlass mechanism cannot support this function without them." It now appears likely then that strengthening the intrinsic muscles of the foot would indeed improve the power and stability of the MTPJs at propulsion. Not only that, it would also appear likely that their strengthening will reduce loads on the plantar fascia during propulsion. We now see that we should not ignore the small stabilisers of all joints in assisting the prime movers, whether that be the shoulder, back, hip or foot. Prevention and Healing for Runners as they Age
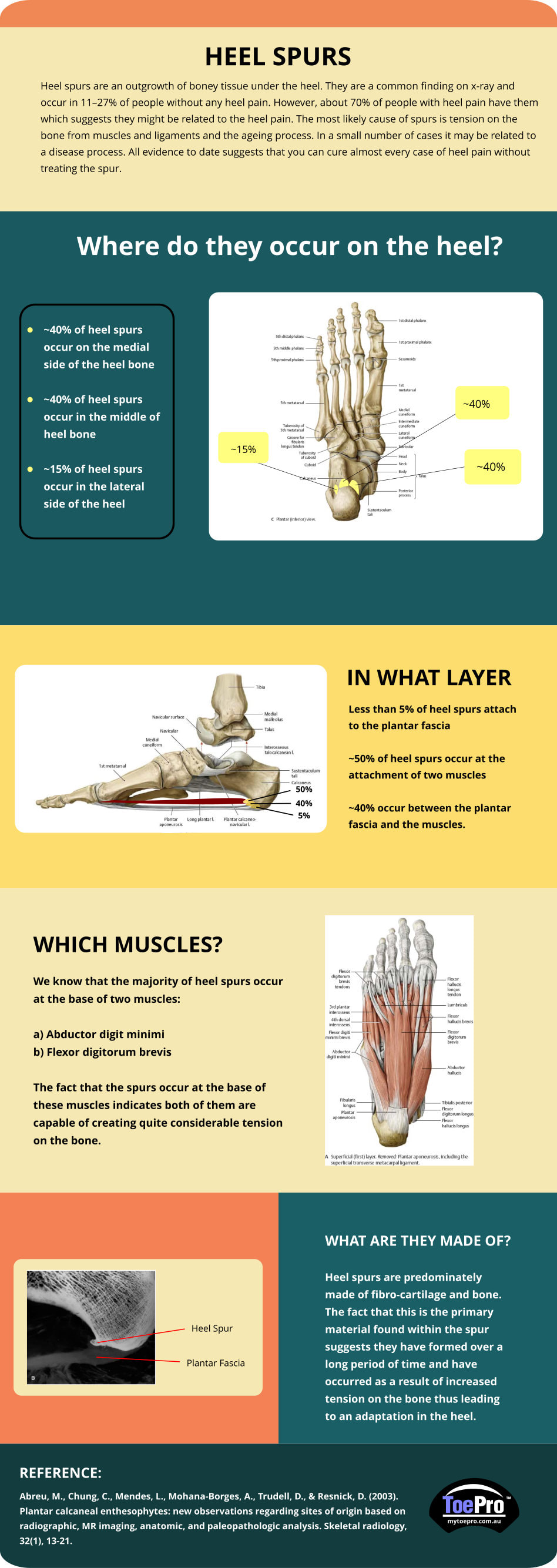
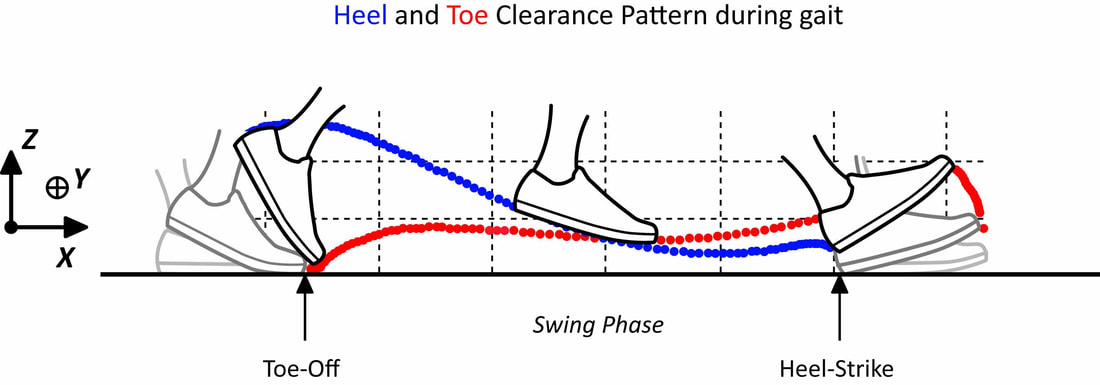
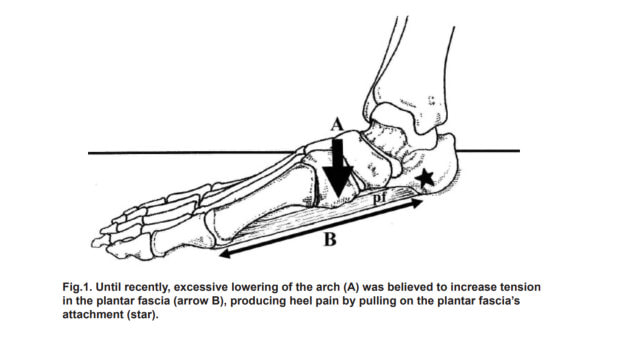
As you age, many things about your body change. Whether you are just leaving your teen years or planning your 100th birthday party, your body is adapting to new circumstances. Keeping it healthy so that you can continue to run as long as you live is a valiant effort. Along the way, there will be years of healing, growing, and learning. Optimally, correct exercise will help prevent the need for long periods of recovery or invasive surgeries. Dr. Tom Michaud has been studying the human body for several decades now. He works as a sports medicine chiropractor, an author, and a researcher. He also creates products for healthcare professionals that help in client examinations. His goal is to provide non-surgical management of injuries, and he specializes in exercise recovery. As you listen to today’s episode of the Running for Real podcast, you will quickly discover that Tom is an expert in his field who has a desire to help and heal others. Listen to the Podcast here. Let’s cut to the chase - if you have an ankle equinus (lack of ankle dorsiflexion) it means that you have an increased chance of developing retracted toes. The greater the equinus the more chance your toes will retract upwards (Cheuy et al., 2015). Your toes retract upwards through increased activity of the extensor muscles (extensor digitorum/hallucis longus/brevis) in response to the restriction in ankle range (most likely due to a short calf). Luckily these extensor muscles do work harder otherwise people with reduced ankle range would trip over their toes during the swing phase of gait. Ground clearance during swing phase is not very large (less than 2 cms for most people depending on height) (Winter, 1992). The downside of the increased extensor activity is it causes greater and greater hyperextension of the MTPJs and makes it harder for the intrinsics to keep the toes straight. During propulsion the lumbricals and interossei become ineffective in stabilising the toes and all we have left are the extrinsic flexors (Flexor digitorum longus which causes the toes to claw without the work of the intrinsics). Therefore, to stop this process we can’t just focus on intrinsic muscle strengthening. The fault in many cases can be the reduced range at the ankle joint (especially in diabetes). For the most part, patients with this limitation primarily have calf weakness and subsequent shortening (they go hand in hand e.g. if you immobilize the calf, it weakens and shortens itself to maintain a healthy length-tension relationship) (DiGiovanni et al., 2002). In diabetes the restriction is in combination with AGE’s (Advanced Glycation End products) which essentially decreased the flexibility of collagen (Rao et al., 2006). To get the best and most effective result for our patients we need to ask them to strengthen their calf muscles by performing an eccentric calf loading program. Eccentric strengthening of muscles in a lengthened position promotes greater strength and length by promoting the physiological process of sarcomerogenesis (Lynn and Morgan, 1994), essentially a process by which the muscle makes itself longer by adding on sarcomeres in series. Once you have done exercise in this way for a few months you will end up with an increased muscle resting length which will return some if not all the lost range in the ankle joint. In doing so you have reduced the need for the extensor muscles to work so hard to clear the ground. In return the patient will have improved range and power in propulsion which will have added benefits for hip and knee function. This is also by far a more effective program than stretching the calf muscles which will only offer short term benefits. Essentially using the ToePro to perform calf eccentric exercises combined with the intrinsic strengthening aspect will give patients a very effective approach to maximising their potential to improve range and improve toe alignment and strength. When do we call it quits? The problem that will raise its head very quickly for patients is that if they have walked in this way for a long period of time the flexion deformity they have developed in their toes may have become fixed. The calf exercises will still be effective in improving the ankle range if the equinus is due to the tightened calf muscles. It will also reduce the risk of further progression of the deformity and should therefore be recommended and most likely will benefit more proximal joints. It would not be unreasonable to recommend stretching of the shortened extensors passively (by say the hands, or by sitting on top of your feet with your feet maximally plantarflexed beneath you) or even to recommend strengthening the extensor tendons in a lengthened position also. The practitioner can also perform mobilisation and manipulation of both the ankle and toes to improve their range. References Cheuy, V. A. et al. (2015) ‘Muscle and Joint Factors Associated with Forefoot Deformity in the Diabetic Neuropathic Foot’, Foot and Ankle International, 37(5), pp. 514–521. doi: 10.1177/1071100715621544. DiGiovanni, C. W. et al. (2002) ‘Isolated gastrocnemius tightness’, Journal of Bone and Joint Surgery - Series A, 84(6), pp. 962–970. doi: 10.2106/00004623-200206000-00010. Lynn, R. and Morgan, D. L. (1994) ‘Decline running produces more sarcomeres in rat vastus intermedius muscle fibers than does incline running.’, Journal of applied physiology (Bethesda, Md. : 1985), 77(3), pp. 1439–1444. doi: 10.1152/jappl.1994.77.3.1439. Rao, S. R. et al. (2006) ‘Increased passive ankle stiffness and reduced dorsiflexion range of motion in individuals with diabetes mellitus’, Foot and Ankle International, 27(8), pp. 617–622. doi: 10.1177/107110070602700809. Winter, D. A. (1992) ‘Foot Trajectory in Human Gait: A Precise and Multifactorial Motor Control Task’, Physical Therapy. Oxford University Press, 72(1), pp. 45–53. doi: 10.1093/ptj/72.1.45. The creator of the ToePro Dr Tom Michaud has released his own paper on the management of heel pain (plantar fasciitis).
"Each year, nearly 2 million Americans seek medical attention for a painful heel. In the US alone, the annual economic cost for managing this common condition is in excess of $300 million. Until recently, it was believed the most common cause of heel pain was an over-pronated foot...." Read the full article here. INCREASING STRENGTH OF INTRINSIC FOOT MUSCLES IN DIABETES WITH PERIPHERAL NEUROPATHY One component of diabetic foot disease is intrinsic muscle wasting – when it is present it is often referred to as the "intrinsic minus foot". The intrinsic minus foot is often discussed as an end stage change which occurs because of, or in addition to, long standing neuropathy and peripheral arterial disease. So, in the minds of many practitioners it is viewed as an inevitable, unfortunate change which sits at the top of a number of other problems in the latter stages of diabetic foot disease. In fact, intrinsic atrophy is one of the earliest changes in diabetic foot disease, occurs often long before peripheral neuropathy and vascular disease and is possibly one of the most important and now known to be reversible changes in the diabetic foot (Greenman et al., 2005; Höhne et al., 2012). However, in the minds of both practitioners and patients they are often more worried about peripheral neuropathy and vascular disease than muscle and structural changes. They often believe that these are the changes that herald the major risk for diabetic ulceration.
This is not the case for majority of people with diabetes. We know that the structural changes in the foot are significant predictors of ulceration and in fact are the predominant changes which lead to ulceration for most people (Holewski et al., 1989; Mueller et al., 2003). Essentially the structural changes in the foot – stiffening and clawing of toes - predict the high pressures under the forefoot. Without these changes you are unlikely to get the high forces which crush and injure foot tissues. If this is combined with a loss of sensation so you are unable to feel the crushing, or if you have a significant reduction in blood supply you cannot repair the crushed tissues. These later problems then escalate the risk significantly. To put it another way, if a patient does not develop stiffening and clawing of toes then they do not have the same level of crushing forces under their foot and if these forces are absent it is less of a concern when the patient develops neuropathy or a lack of blood supply. Our biggest priorities as practitioners is to do everything in our power to educate patients to begin the process of maintaining strength and mobility, especially of the toes, so they stop or reduce their risk of developing high forefoot pressures (Sartor et al., 2014). There is now a growing body of research which demonstrates we can indeed reverse muscle atrophy in the forefoot, improve mobility of toes and when we do so we can reduce plantar pressures which crush the tissues under the foot (Allet et al., 2010; Sartor et al., 2014; Kanchanasamut and Pensri, 2017). An excellent example of such research was published by Höhne et al in Cologne, Germany (Höhne et al., 2012). Fourteen diabetic patients with only 30% of normal toe flexor strength performed toe flexor training with 70% of the maximal voluntary isometric contraction on for eight weeks, 3 days per week, 4 sets per session for twelve repetitions (3s loading/ 3s relaxation). The participants were divided into groups of either those with or without neuropathy. Seven had neuropathy, seven without neuropathy. The maximum strength of the toes was measured before and after the intervention and the volume of the intrinsic foot muscles was examined before and after the intervention using MRI. All patients improved strength, with the average increase being a staggering 55% increase in just 8 weeks. The intervention took only 10 minutes roughly 3 times per week and could be performed at home with little difficulty. In addition, there were no instructions to utilise their strength in everyday activities. So the strength gains can only be attributed to intervention of a total of 30 minutes per subject per week. Furthermore, the MRI results showed an average increase of 5% muscle bulk in just those 8 weeks. We can begin to understand the possible benefits if we were to perform these exercises every day, in a functional position, with functional loads (bodyweight) combined with daily use activities to create positive carry over. References Allet, L. et al. (2010) ‘An exercise intervention to improve diabetic patients’ gait in a real-life environment’, Gait and Posture. Elsevier B.V., 32(2), pp. 185–190. doi: 10.1016/j.gaitpost.2010.04.013. Greenman, R. L. et al. (2005) ‘Foot small muscle atrophy is present before the detection of clinical neuropathy.’, Diabetes care. American Diabetes Association, 28(6), pp. 1425–30. doi: 10.2337/DIACARE.28.6.1425. Höhne, A. et al. (2012) ‘Increased Strength of Intrinsic Foot Muscles in Diabetes and Peripheral Neuropathy’, Journal of Biomechanics. Elsevier Ltd, 45(1), p. S201. doi: 10.1016/S0021-9290(12)70202-6. Holewski, J. J. et al. (1989) ‘Prevalence of foot pathology and lower extremity complications in a diabetic outpatient clinic.’, Journal Of Rehabilitation Research And Development, 26(3), pp. 35–44. Available at: http://www.ncbi.nlm.nih.gov/pubmed/2666642. Kanchanasamut, W. and Pensri, P. (2017) ‘Effects of weight-bearing exercise on a mini-trampoline on foot mobility, plantar pressure and sensation of diabetic neuropathic feet; a preliminary study’, Diabetic Foot and Ankle. Taylor & Francis, 8(1). doi: 10.1080/2000625X.2017.1287239. Mueller, M. J. et al. (2003) ‘Forefoot structural predictors of plantar pressures during walking in people with diabetes and peripheral neuropathy’, Journal of Biomechanics, 36(7), pp. 1009–1017. doi: 10.1016/S0021-9290(03)00078-2. Sartor, C. D. et al. (2014) ‘Effects of strengthening, stretching and functional training on foot function in patients with diabetic neuropathy: Results of a randomized controlled trial’, BMC Musculoskeletal Disorders, 15(1), pp. 1–13. doi: 10.1186/1471-2474-15-137. |
AuthorMatt Dilnot is a Podiatrist working in the Eastern Suburbs of Melbourne, Victoria. Archives
May 2020
Categories |






 RSS Feed
RSS Feed